Vitamin D3 is best known for general health because it helps your body absorb calcium. The absorption of calcium is only the tip of the iceberg for the uses and functions of Vitamin D in your body. It’s estimated that 40-85% of the population is deficient in vitamin D, which plays a central role in everything from regulating mood to modulating immune cells in the body and beyond. Not only that, but it’s one of the few nutrients that’s difficult to get from food sources alone, making supplementation absolutely necessary in many cases.
So what’s the difference between vitamin D vs. D3 and D2? And what is vitamin D3 good for?
What Is Vitamin D3?
Vitamin D3, as a nutritional supplement is known as cholecalciferol. It is a fat-soluble vitamin that is involved in bone health, immune function, cell growth and more. It’s one of the few nutrients that your body is able to produce on its own through the skin cells in response to sun exposure. It can also be obtained through several vitamin D food sources and supplements as well.
Unfortunately, vitamin D deficiency is a common issue, and certain groups are at a higher risk of deficiency. In particular, older adults, those who get limited sun exposure, and people who are overweight/obese or have darker skin are at an increased risk.
Vitamin D3 vs. Vitamin D2
Vitamin D is available in two forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D3 is primarily found in animal foods, such as fish, liver, eggs and cod liver oil. Meanwhile, vitamin D2 is mostly in mushrooms and fortified foods, such as cereal.
Both are also available in supplement form as well. The biggest difference between vitamin D2 vs. D3 actually lies in the way that they are metabolized in the body. In fact, one study published in the Journal of Endocrinology and Metabolism found that vitamin D3 was nearly twice as effective at increasing vitamin D levels in the blood compared to vitamin D2.
For this reason, it’s generally recommended to select a vitamin D3 supplement whenever possible to optimize absorption and get the most bang for your buck. Taking a vitamin D3 supplement is an effective way to boost calcium absorption, promote bone health, support weight management and more.
Benefits of Vitamin D3 Supplementation
According to the NIH, Vitamin D has other roles in the body, including reduction of inflammation as well as modulation of such processes as cell growth, neuromuscular and immune function, and glucose metabolism. Many genes encoding proteins that regulate cell proliferation, differentiation, and apoptosis are modulated in part by vitamin D. Many tissues have vitamin D receptors, and some convert 25(OH)D to 1,25(OH)2D. It is well documented that Vitamin provides the following benefits:
1. Weight management is one of the most popular uses of vitamin D3. Interestingly enough, studies actually show that vitamin D levels tend to be lower in people with higher amounts of body fat. Some research also suggests that supplementing with vitamin D could enhance weight loss and bump up fat-burning. For example, a study conducted by the Department of Social and Preventive Medicine at Laval University in Canada demonstrated that supplementing with calcium and vitamin D increased weight loss and fat loss compared to a control group.
2. Boosts Bone Strength: Vitamin D is absolutely essential when it comes to bone health. In fact, one of the most serious vitamin D3 deficiency symptoms in children is rickets, a condition characterized by a softening and weakening of the bones. One of the main ways that vitamin D boosts bone strength is by promoting the absorption of calcium, which is essential to maintaining skeletal integrity. Plus, it’s also involved in the metabolism of phosphorus, another key mineral that is important to bone health.
3. Improves Immune Function: One of the most impressive benefits of vitamin D3 is its ability to enhance immunity and protect against infection. Not only can a deficiency in this important micronutrient slow wound healing and increase the risk of infection, but vitamin D3 is also integral to the function of immune cells in the body. According to one study by Dr. Ginde and colleagues, lower levels of serum vitamin D are actually associated with the a higher risk of recent respiratory tract infections, demonstrating just how crucial this vitamin is for immunity.
A new report by Spanish researchers at the Hospital del Mar in Barcelona has added evidence to the benefits of D3 supplements as a treatment for coronavirus patients. Their study of 930 COVID-19 patients found that those who received the supplement, rather than a placebo, saw a “reduced mortality of more than 60%,” study authors wrote. These patients were additionally 80% less likely to require intensive care at the hospital. Just 36 of the 551 patients who took D3 died from the coronavirus. Meanwhile, the control group of 379 patients lost 57 to the disease. Furthermore, just 5% of the cohort taking D3 were admitted to the ICU.
4. Glucose Management/Metabolic Support: It has been reported as early as the 1980s that vitamin D deficiency inhibits pancreatic secretion and turnover of insulin, resulting in impaired glucose tolerance. A study of 83,779 women with no history of diabetes over 2-4 years showed that a combined daily intake of >1200 mg calcium and >800 IU vitamin D was associated with 33% lower risk of type 2 diabetes as compared with a daily intake of less than 600 mg of calcium and less than 400 IU of vitamin D. Another study on 10,366 children in Finland over 31 years indicated that 2000 IU of vitamin D per day during their first year of life can reduce the risk of type 1 diabetes by approximately 80%. Another feature of Vitamin D in diabetes is that is has been shown to reduce inflammation, which is a major process in inducing insulin resistance.
5. Cardiovascular Health: Millions of people are affected by hypertension worldwide. Growing evidence in recent years suggests that vitamin D has an important association with blood pressure. Reduced blood pressure has been found in people taking oral supplementation of vitamin D.
6. Enhances Mental Health: Some research shows that vitamin D could be beneficial for boosting mental health and brain power. Studies have found that vitamin D status could potentially be linked to issues like depression, anxiety, Alzheimer’s disease, bipolar disorder and schizophrenia. What’s more, one study conducted by the Washington University School of Medicine even showed that low levels of vitamin D were tied to low mood and impaired cognitive performance in older adults.
7. May Help Fight Cancer Cells: Although research is still limited on exactly how vitamin D3 can impact cancer growth in humans, in vitro research suggests that it may affect several aspects of cancer development, including tumor growth and cell death. Other studies have found that vitamin D deficiency may be linked to a higher risk of certain types of cancer, including breast, prostate, colorectal, ovarian, kidney and stomach cancers. However, further research is still needed to determine whether other factors may also be involved besides vitamin D3 levels.
Normal versus Optimal Vitamin D levels
Based on years of patient testing and data analysis, the NIH and laboratory report reference range to reflect that Vitamin D values between 20-80 ng/mL are representative of a normal patient population
This of course raises the issue: is normal the same thing as optimal? Not necessarily. The Vitamin D Council places the ideal level between 40 and 80 ng/mL with levels below 20 ng/mL as deficient. The Endocrine Society has a Clinical Practice Guideline on the evaluation, treatment, and prevention of vitamin D deficiency. This guideline recommends a minimum vitamin D level of 20 ng/mL, but to guarantee sufficiency they recommend between 30 and 50 ng/mL for both children and adults. In contrast, the Vitamin D Council states that even levels between 30 and 40 ng/mL are still not quite sufficient. On the other end of the spectrum, results that fall between 80 and 100 ng/mL are not achievable naturally; that is, they are only reached with some form of vitamin D supplementation.
From the NIH:
Researchers have not definitively identified serum concentrations of 25(OH)D associated with deficiency (e.g., rickets), adequacy for bone health, and overall health. After reviewing data on vitamin D needs, an expert committee of the Food and Nutrition Board (FNB) at the National Academies of Sciences, Engineering, and Medicine (NASEM) concluded that people are at risk of vitamin D deficiency at serum 25(OH)D concentrations less than 30 nmol/L (12 ng/mL; see Table 1 for definitions of “deficiency” and “inadequacy”) [1]. Some people are potentially at risk of inadequacy at 30 to 50 nmol/L (12–20 ng/mL). Levels of 50 nmol/L (20 ng/mL) or more are sufficient for most people. In contrast, the Endocrine Society stated that, for clinical practice, a serum 25(OH)D concentration of more than 75 nmol/L (30 ng/mL) is necessary to maximize the effect of vitamin D on calcium, bone, and muscle metabolism [11,12]. The FNB committee also noted that serum concentrations greater than 125 nmol/L (50 ng/mL) can be associated with adverse effects [1] (Table 1).
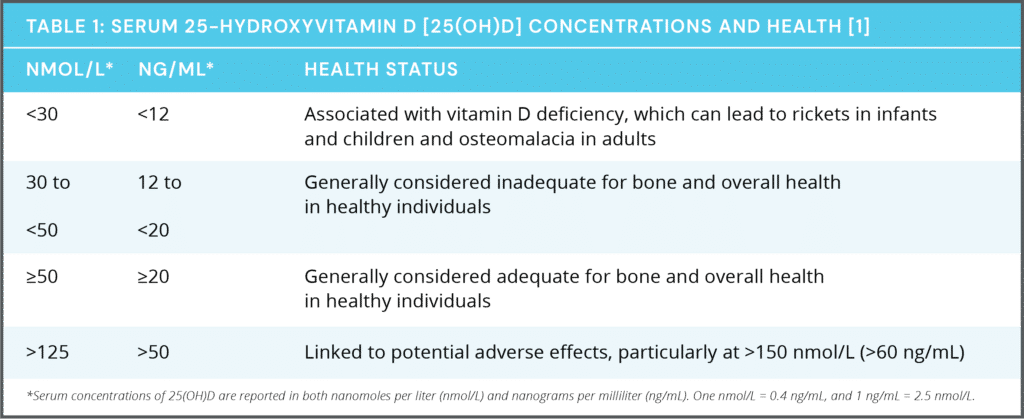
Optimal serum concentrations of 25(OH)D for bone and general health have not been established because they are likely to vary by stage of life, by race and ethnicity, and with each physiological measure used [1,13,14]. In addition, although 25(OH)D levels rise in response to increased vitamin D intake, the relationship is nonlinear [1]. The amount of increase varies, for example, by baseline serum levels and duration of supplementation.
From this summary, you can easily see why Vitamin D deficiency in the world population ranges between 40-85%: It depends on what levels are normal or optimal.
Recommended Vitamin D3 Intakes (NIH):
Intake recommendations for vitamin D and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by expert committees of NASEM [1]. DRI is the general term for a set of reference values used for planning and assessing nutrient intakes of healthy people. These values, which vary by age and sex, include:
- Recommended Dietary Allowance (RDA): Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- Adequate Intake (AI): Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an RDA.
- Estimated Average Requirement (EAR): Average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals.
- Tolerable Upper Intake Level (UL): Maximum daily intake unlikely to cause adverse health effects.
An FNB committee established RDAs for vitamin D to indicate daily intakes sufficient to maintain bone health and normal calcium metabolism in healthy people. RDAs for vitamin D are listed in both micrograms (mcg) and international units (IU); 1 mcg vitamin D is equal to 40 IU (Table 2). Even though sunlight is a major source of vitamin D for some people, the FNB based the vitamin D RDAs on the assumption that people receive minimal sun exposure [1]. For infants, the FNB committee developed AIs based on the amount of vitamin D that maintains serum 25(OH)D levels above 20 ng/mL (50 nmol/L) and supports bone development.
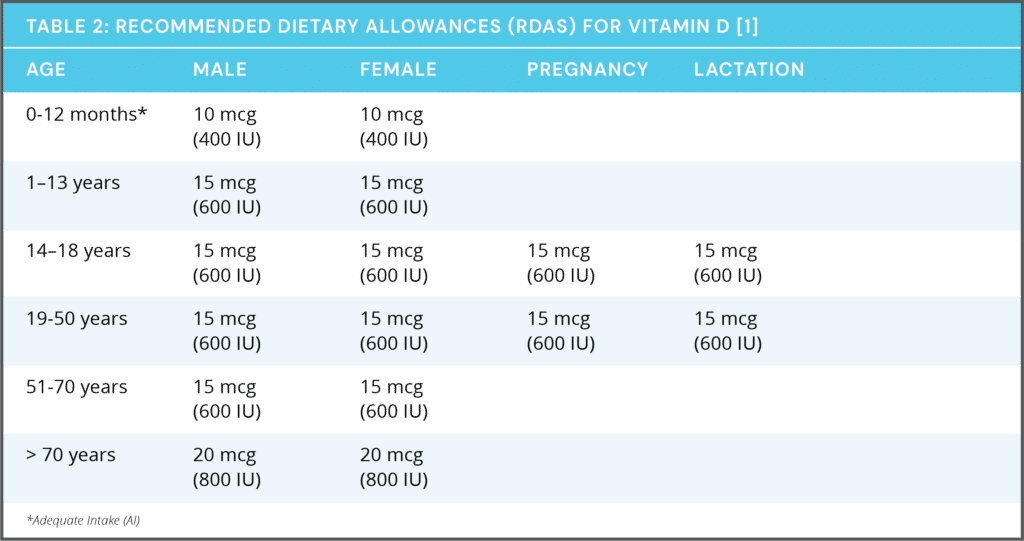
Many other countries around the world and some professional societies have somewhat different guidelines for vitamin D intakes [15]. These differences are a result of an incomplete understanding of the biology and clinical implications of vitamin D, different purposes for the guidelines (e.g., for public health in a healthy population or for clinical practice), and/or the use in some guidelines of observational studies in addition to randomized clinical trials to establish recommendations [9,15]. The Endocrine Society states, for example, that to maintain serum 6 25(OH)D levels above 75 nmol/L (30 ng/mL), adults might need at least 37.5 to 50 mcg (1,500–2,000 IU)/day of supplemental vitamin D, and children and adolescents might need at least 25 mcg (1,000 IU)/day [11]. In contrast, the United Kingdom government recommends intakes of 10 mcg (400 IU)/day for its citizens aged 4 years and older [16].
Vitamin D Toxicity
What is vitamin D toxicity? Should I be worried about taking supplements? Answer From Katherine Zeratsky, R.D., L.D. Mayo Clinic:
Vitamin D toxicity, also called hypervitaminosis D, is a rare but potentially serious condition that occurs when you have excessive amounts of vitamin D in your body.
Vitamin D toxicity is usually caused by large doses of vitamin D supplements — not by diet or sun exposure. That’s because your body regulates the amount of vitamin D produced by sun exposure, and even fortified foods don’t contain large amounts of vitamin D.
The main consequence of vitamin D toxicity is a buildup of calcium in your blood (hypercalcemia), which can cause nausea and vomiting, weakness, and frequent urination. Vitamin D toxicity might progress to bone pain and kidney problems, such as the formation of calcium stones.
Treatment includes stopping vitamin D intake and restricting dietary calcium. Your doctor might also prescribe intravenous fluids and medications, such as corticosteroids or bisphosphonates.
Taking 60,000 international units (IU) a day of vitamin D for several months has been shown to cause toxicity. This level is many times higher than the U.S. Recommended Dietary Allowance (RDA) for most adults of 600 IU of vitamin D a day.
Contraindications for taking Vitamin D3
You should not use cholecalciferol if you have had an allergic reaction to vitamin D, or if you have:
- high levels of vitamin D in your body (hypervitaminosis D);
- high levels of calcium in your blood (hypercalcemia); or
- any condition that makes it hard for your body to absorb nutrients from food (malabsorption).
Absorption and Bioavailability of Vitamin D3
Cholecalciferol is a lipophilic compound (fat soluble) that is converted in the liver to calcifediol (25-hydroxycholecalciferol); ergocalciferol is converted to 25-hydroxyergocalciferol. These two vitamin D metabolites (called 25-hydroxyvitamin D or 25(OH)D) are measured in serum to determine a person’s vitamin D status. In more general terms, Vitamin D3 is a non-polar lipid with poor bioavailability due to its low solubility in aqueous fluids of gastrointestinal trac.
References
Berridge MJ. Vitamin D deficiency and diabetes. Biochem J. 2017 Mar 24;474(8):1321-1332. doi: 10.1042/BCJ20170042. PMID: 28341729.
Hollander D, Muralidhara KS, Zimmerman A. Vitamin D-3 intestinal absorption in vivo: influence of fatty acids, bile salts, and perfusate pH on absorption. Gut. 1978 Apr;19(4):267-72. doi: 10.1136/gut.19.4.267. PMID: 25826; PMCID: PMC1411923.
Maurya VK, Aggarwal M. Factors influencing the absorption of vitamin D in GIT: an overview. J Food Sci Technol. 2017 Nov;54(12):3753-3765. doi: 10.1007/s13197-017-2840-0. Epub 2017 Sep 23. PMID: 29085118; PMCID: PMC5643801.
Zhang, R., Naughton, D.P. Vitamin D in health and disease: Current perspectives. Nutr J 9, 65 (2010). https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-9-65
Hanafy AS, Elkatawy HA. Beneficial Effects of Vitamin D on Insulin Sensitivity, Blood Pressure, Abdominal Subcutaneous Fat Thickness, and Weight Loss in Refractory Obesity. Clin Diabetes. 2018 Jul;36(3):217-225. doi: 10.2337/cd17-0099. PMID: 30078941; PMCID: PMC6053848.
Anglin RE, Samaan Z, Walter SD, McDonald SD. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry. 2013 Feb;202:100-7. doi: 10.1192/bjp.bp.111.106666. PMID: 23377209.
Ginde AA, Mansbach JM, Camargo CA Jr. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2009 Feb 23;169(4):384-90. doi: 10.1001/archinternmed.2008.560. PMID: 19237723; PMCID: PMC3447082.
Vitamin D. Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
Zeratsky, Z, What is vitamin D toxicity? Should I be worried about taking supplements? Mayo Clinic Online. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/basics/nutrition-basics/hlv-20049477